Neuromuscular disorder (NMD) is a broad term for a range of conditions. It affects the functioning of the muscles causing progressive muscle weakness. Everyday activities become more difficult. Neuromuscular disorders can be caused by a problem
No matter what the cause, they all have one thing in common, progressive muscle wasting.
Click here for more information on the Scottish Muscle Network (SMN) and Muscular Dystrophy UK.
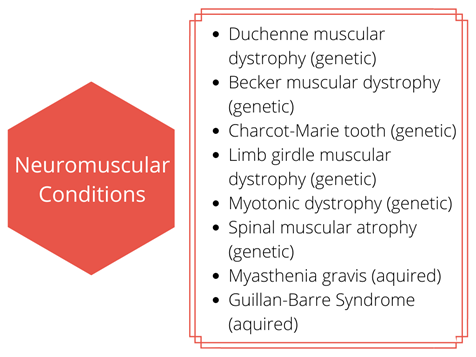
There are over 70 neuromuscular disorders that we know of. Many other neuromuscular conditions are still unknown despite major advances in the world of genetics. Neuromuscular disorders can be diagnosed in babies, infants, children, adolescents and adults. About a third of patients with a muscle disorder will not have a specific name for their condition. This is because the genetic cause has yet to be determined. Neuromuscular disorders can run in families (genetic) or occur at a point through life (acquired).
You may already have contact with a physiotherapist in the hospital (acute service). If you need physiotherapy at home or in school community specialist children’s service can provide this. We work together with our colleagues from the hospital. You can also self-refer to physiotherapy if you need advice.
 With neuromuscular disorders your muscles will be weaker. The muscles involved will vary depending on your diagnosis and can happen during childhood or later in life. You may find some activities more difficult than others or require some assistance. In some neuromuscular disorders, it takes less stress to damage a muscle and the repair may take longer. As the muscle, or nerve supplying the muscle is damaged (depending upon the condition), it can be more difficult to build the muscle or make it stronger. Muscles impact every aspect of our life because muscles mean movement and if the movement is interrupted it will affect our posture, energy, the way we walk or move around. In some cases, you may experience some discomfort caused by the weakness which can affect your joints. If we don't have internal muscle strength, we will need help with external support such as Orthotics.
With neuromuscular disorders your muscles will be weaker. The muscles involved will vary depending on your diagnosis and can happen during childhood or later in life. You may find some activities more difficult than others or require some assistance. In some neuromuscular disorders, it takes less stress to damage a muscle and the repair may take longer. As the muscle, or nerve supplying the muscle is damaged (depending upon the condition), it can be more difficult to build the muscle or make it stronger. Muscles impact every aspect of our life because muscles mean movement and if the movement is interrupted it will affect our posture, energy, the way we walk or move around. In some cases, you may experience some discomfort caused by the weakness which can affect your joints. If we don't have internal muscle strength, we will need help with external support such as Orthotics.
Muscles help us speak and breathe so we may need additional help in these areas depending upon our condition (click here for more information on Speech & Language Therapy).
Muscle Fatigue is common in neuromuscular disorders. Fatigue is when your muscles become tired and/or sore and you feel a lack of energy.
Fatigue in some neuromuscular conditions can be:
It is important to be aware of when your muscles become tired and rest as too much activity can take longer to recover from. It is important to pace your activity. Pacing means slowing down and taking your time, spacing out the activities you have to do or changing to a different activity to give your muscles a rest. You may find walking becomes difficult. Depending on your condition you may require a walking aid or a wheelchair to help you move around or to manage your energy for periods throughout the day or all of the time.
Physiotherapists can help you in many of these areas with specific advice on muscle weakness and fatigue management. We can do this by looking at posture and advising on energy conservation to help you do the things that matter most. We want to make sure you grow well and will help you find ways of keeping your muscles as strong as they can be and may give you exercises and stretches to stop them from becoming tight. If they are tight we can look for ways to help keep them where they are and prevent further tightness.
If you require physiotherapy the programme we give you will be appropriate for your condition.
 Breathing involves the respiratory muscles. This includes the diaphragm (the big muscle under the lungs) and the muscles between the ribs (the intercostals). There are some other muscles but it is these two muscle groups that are the main breathing muscles. They can become weaker over time the same as other muscles in the body affected by muscle conditions. This can cause “under breathing”. This is when our muscles cannot open our lungs fully to take in and breathe out enough air effectively. It is not that there is anything wrong with the lungs. The lungs still work well. But the muscles that control the amount (or volume) of air that goes in and out of our lungs cannot do this as well as they used to.
Breathing involves the respiratory muscles. This includes the diaphragm (the big muscle under the lungs) and the muscles between the ribs (the intercostals). There are some other muscles but it is these two muscle groups that are the main breathing muscles. They can become weaker over time the same as other muscles in the body affected by muscle conditions. This can cause “under breathing”. This is when our muscles cannot open our lungs fully to take in and breathe out enough air effectively. It is not that there is anything wrong with the lungs. The lungs still work well. But the muscles that control the amount (or volume) of air that goes in and out of our lungs cannot do this as well as they used to.
The breathing muscles are used to help us cough effectively. This allows secretions (mucous) to be cleared from the lungs. When these muscles become weak an ineffective cough results. Secretions are then prevented from being cleared from the lungs. In some cases, the secretions can block the small airways in our lungs. If the airways are blocked the secretions cannot move into the larger airways for us to cough them out and clear our lungs. If secretions are not being cleared they can cause infection. You need help from your doctor and physiotherapist to get everything moving again. Respiratory issues in muscle conditions can vary a lot between children and each condition.
 Keeping healthy and taking some precautions can help keep your chest clear. This can minimise your chances of getting a chest infection. The following advice can help you look after yourself:
Keeping healthy and taking some precautions can help keep your chest clear. This can minimise your chances of getting a chest infection. The following advice can help you look after yourself:

The respiratory system (breathing muscles and lungs) can be assessed by a physiotherapist. A respiratory assessment by a physiotherapist may involve listening to your chest and feeling the movement of your chest to assess your breathing pattern.

If you develop any of the following symptoms it is important that you visit your GP. Follow guidance from your physiotherapist on your respiratory plan if you have one.
 If you develop any of the symptoms mentioned above it is important to contact your GP as they could be signs of an infection.
If you develop any of the symptoms mentioned above it is important to contact your GP as they could be signs of an infection.
If you have a physiotherapy respiratory programme and have any problems or questions about it you can contact your community physiotherapist if you have one or alternatively contact the physiotherapists at the hospital.
Falls are common in people who have a neuromuscular disorder. A combination of the following can put you at greater risk:
It is important to try and reduce the chances of tripping and falling. Injury after a fall can lead to prolonged periods of immobility. This can lead to muscle weakness and difficulty getting back on your feet again. People are more likely to have a fall in unfamiliar surroundings and when they are concentrating on other things. It is important to look in the direction you are walking to negotiate obstacles and other areas of risk. Sudden changes in direction and speed can cause you to overbalance. Walking aids can help with this if needed. They will give those around you a visual prompt that you might need a bit more personal space. Walking frames, crutches and the use of a wheelchair can all help with safer mobility. They reduce the chances of fatigue (tiredness) and falling. Ankle splints and other types of ankle supports are particularly helpful when a ‘drop foot’ is present. A ‘drop foot’ is the inability to lift your foot and toes properly when walking. This can increase the chance of your foot or toe catching on an object and causing you to trip up. Outdoor surfaces are dangerous due to uneven surfaces. It is very important to wear ankle support if one is needed. It is important to talk to your physiotherapist about the best walking aid for you. You can also discuss with them supports that could help your personal needs.
Making simple changes at home and planning ahead is useful. Removing rugs and toys scattered on the floor reduces the risk of tripping over them. An Occupational Therapist can help with more specialist home equipment for your needs. Your physiotherapist or doctor can refer you to them.
If a fall occurs, and there are ongoing concerns, if it is appropriate a Physiotherapist can assist in assessing your ability to get back up from the floor. They can discuss with you and your parents/carer handling methods to assist with this.
Scoliosis is a curvature of the spine and is common in many neuromuscular disorders. The curvature progresses (increases) over time more frequently in neuromuscular disorders due to muscle weakness.
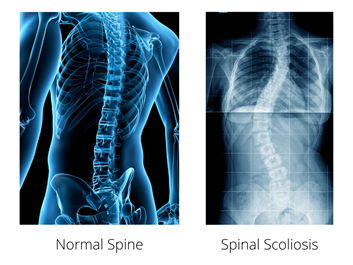
Signs of scoliosis include:
Once the curve gets to a certain stage it can cause discomfort. To reduce the progression of scoliosis it is important that you have a 24-hour postural management programme in place to support your body in a good position. You can speak to your physiotherapist about this. Click here for more information on Postural Management.
If you have scoliosis you can be more at risk of chest infections. Keeping the spine straighter will mean that it is easier to look after your chest during chest infections.
You may be offered surgery to help straighten your back if the curve is seen to be changing. Once the curve reaches a certain angle, we know that the curve will continue to get worse. When the curve becomes worse, it can make sitting more difficult and you may feel more uncomfortable. If this is something that is needed it will be discussed with the specialist doctors at the hospital, you, and your parents or caregivers.
If you do require surgery then your postural needs will change after this. This will be discussed before your surgery and your physiotherapist and occupational therapist can give you advice on any equipment you already have that will need to be adjusted for example if you are hoisted or have a wheelchair, home seating or a shower chair.
You should discuss when you can go back to your usual activity with your spinal surgeon. It is generally recommended that moderate activity should be stopped until you have healed. Your surgeon will be able to give you more information on this as each person is different and it will depend on the level of surgery you have had and how quickly you heal.
 In neuromuscular conditions, there are several factors that can cause pain. Weakening muscles reducing support to the joints in the body can result in poor postures. It becomes more difficult to change your position. This can lead to pain and discomfort. Depending on your condition muscle pain can also be caused by inflammation and tight muscles.
In neuromuscular conditions, there are several factors that can cause pain. Weakening muscles reducing support to the joints in the body can result in poor postures. It becomes more difficult to change your position. This can lead to pain and discomfort. Depending on your condition muscle pain can also be caused by inflammation and tight muscles.
There are different ways to manage pain. This may involve different health professionals. Physiotherapists can look at posture and movement. They can see what may be the cause of your pain. By looking at how you position yourself when you sleep, sit and stand and the way in which you move around in your daily activities can also help.
Changing the way in which you do certain tasks may help reduce your level of pain in the short term. It can help you maintain manageable pain levels in the long term. Energy conservation is important to reduce the amount of strain placed on your body which will in turn help reduce pain. Methods used to help control pain include the use of aids and adaptations, relaxation and ensuring a healthy lifestyle. You can speak with your doctor about the use of pain medication if required. The use of pain medication should be closely monitored by your doctor or nurse. This will ensure it does not interfere with any other medications you are already on.
Activities are good for everyone. We all have our likes and dislikes. You can decide what you enjoy best.

Click here for some ideas, you may require some advice from a health professional on what is appropriate for your neuromuscular condition.